Microfluidic chips enhance the semen analysis and sperm selection processes
At least 50 million couples are suffering from infertility worldwide. The sperm quality and sperm concentration reduction due to environmental and genetic reasons have also given rise to concerns in many European and American countries facing high infertility rates that in turn prevents population sustainability.

Clinics all around the world are using Assisted Reproductive Technologies (ARTs) to overcome the infertility issue and help couples achieve their dream of having a child. However, not all attempts are successful. The success rate of these methods has plateaued at nearly 33%. The ART methods such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) involve placing a selected group of sperms near the egg or directly injecting it to the egg. An important step in these technologies is sperm selection. In the female reproductive organ, a sperm has to take a long journey to reach the egg. However, a concern in ARTs is that this process is that all these natural barriers are removed. Therefore, the selected sperm might not have the required quality causing failure in the process. More advanced technologies such as microfluidics can improve the sperm analysis and sperm selection process and increase the success rate.
Additionally, semen analysis is of crucial importance for diagnosing infertility. The quality of the semen can be influenced by a number of factors including sperm count, DNA integrity, and motility. Current techniques for semen analysis are time-consuming and require well-trained technicians. Easier and faster tests and devices for semen analysis can be beneficial for infertility diagnosis.
Microfluidics can boost this process by providing clinicians and researchers with prices, high throughput, and affordable devices for semen analysis and sperm selection. Microfluidics enables researchers and clinicians to select high-quality sperms at a higher throughput than conventional methods. Microfluidic chips can be automated to remove the human error in manual processes.
Additionally, microfluidics allows for single-sperm selection and analysis. In severe cases of infertility where the patient is suffering from very low sperm count, single-sperm microfluidic devices can help in selecting a healthy and motile sperm.
- Microchannels with biologically relevant dimensions (5-300 µm)
- High sensitivity
- Rapid testing
- Low reagent consumption
- 2D and 3D channel designs
- Suitablity for in-home testing
Semen analysis using microfluidic technology
The first step for treatment is diagnosis. Male infertility could be due to low sperm concentration, vitality, motility, and damage to the DNA. Current techniques such as counting chambers, CASA, and SCSA are time-consuming, complicated, prone to operator error, or dependant on expensive laboratory equipment. Additionally, they require the male participant to give a semen sample that causes incompliance in men.
Microfluidic chips are alternatives for conventional manual processes for semen analysis. These screening chips can be disposable and enable in-home screening for patients. Patients undergoing treatment can screen their progress without the need to visiting the doctor in-person. An online software can also inform the doctor of the patient’s conditions.
In general, conventional techniques hinge upon batch analysis of samples. But, microfluidic devices are tunable and can increase the sensitivity and accuracy up to single-sperm resolution.
Many of the ideas published in the literature have the potential to appear on the market with further testing. The market can enjoy these microfluidics chips in both clinical practices and point-of-care applications. The affordability and ease of use make these microfluidics chips a good choice for POC and in-home testing in low-income countries. We, at uFluidix, with more than 10 years of experience in prototyping and custom Microfluidics fabrication are more than happy to discuss your project with you. Please fill out the form below to discuss your inquiry with one of our specialists.
Microfluidic chips for sperm sorting and selection
The IVF and ICSI are two common assisted reproductive technologies. IVF involves placing a pool of sperms near the egg while in ICSI a single sperm is injected to the egg. In both techniques, sperm selection plays a pivotal role. The selection of a motile and a morphologically normal sperm is an integral step in ARTs. A healthy and high-quality sperm with high DNA integrity and proper structure can increase the pregnancy rate and live birth. An incompetent and unhealthy sperm can result in failure in reproduction or affect the health of the offspring.
In the body, the sperm has to undergo a long journey to reach the egg. The difficulty of traveling this path reduces the probability of unhealthy and damaged sperms to reach the egg. However, in the ARTs, this natural process does not exist and can negatively affect the health of the offspring as well as the success rate of the method. Currently, the sperm selection conventions include swim-up technique or density gradient that lack efficiency and the results can vary based on the embryologist’s expertise.
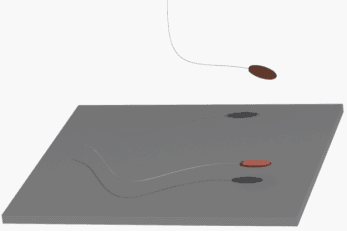
In order to overcome the incompetence of the conventional techniques in mimicking the natural sperm selection process, microfluidic sperm selection chips allow creating more naturally relevant environments leading to the selection of high-quality sperms. The female reproductive organ is very complex. As opposed to the traditional approaches, microfluidic chips and microfluidics devices can be designed to create a bioinspired environment for the sperm to increase the selectivity. The microfluidic chips are often fabricated to mimic the natural environment for the sperms or include microchannels that separate motile and healthy ones from the defected ones.
Current microfluidics chips for sperm selection are either passive or active. In passive devices, the selection process utilizes the sperm motility. The microchannels are designed such that the sperms with higher motility swim to a side channel. In some designs, two streams flow alongside each other; one being the sample and the other a clean buffer. The sperms with high motility swim to the clean buffer. These high-quality sperms are then collected from these channels. Many other passive microfluidics techniques such as spiral channels exist which are listed in the resources section below.
Passive methods for sperm selection mainly focus on the motility of the sperms. Passive microfluidic sperm sorters vary in design. Some of the sperm selection microchips merely race the sperms in a microchannel and collect the selected sperms from the outlet. Other microfluidics based designs can include polycarbonate filters to only allow sperms with high motility pass through the pores. The geometrical features and barriers in the microchannels can also enhance the performance of the chips.
Active sperm selection microfluidic methods require an external source for sorting the sperm. Some known active methods are listed here:
Chemotaxis: Sperms are known to respond to a chemical gradient. Here progesterone (P4) appears to be a major chemoattractant. The chips can be designed such that they provide a chemical gradient for the sperms to attract them towards the desired microchamber or an outlet.
Rheotaxis: Human sperm is responsive to fluid flow. The sperms tend to position themselves against the flow. This has been the context of study for rheotaxis microfluidic chips where a series of interconnected microfluidic channels provide an opportunity for the motile sperms to swim against the flow and be trapped in collection microchambers.
Thermotaxis: Thermotaxis is defined as the movement towards a specific temperature zone in a temperature gradient. It is believed that sperms can respond to a temperature gradient which is the mechanism that allows them to position themselves in the fallopian tube. However, only the capacitated sperms respond to the thermal stimuli. Therefore, they can be separated from the rest using a temperature gradient in a microfluidic chip.
Light-induced electrophoresis: Here, optical tweezers can be employed separate viable sperms. Viable (motile and non-motile) sperms respond differently to the electric field caused by the optical tweezer and can thus be separated. This technique can be of import for ICSI where single sperms are needed and in cases of severe low sperm counts. The optical tweezers are believed not to induce DNA fragmentation.
As opposed to conventional methods, these passive and active microfluidics approaches are centrifuge-free. Thus, the sperms undergo the least damage during the selection process. The throughput is higher and a lower amount of reagents is needed.
There is a significant potential for microfluidic products enabling sperm selection to emerge on the market and be used as powerful tools in fertility clinics. Whether you are a researcher interested in fertility studies or an R&D scientist looking for advancing your current fertility technologies, uFluidix can help you in all stages of the device development, from microfluidic device design and conceptualizing to prototyping and mass manufacturing.
Further Reading
- In vitro fertilization on a single-oocyte positioning system integrated with motile sperm selection and early embryo development
- Rheotaxis-based separation of sperm with progressive motility using a microfluidic corral system
- Selection of functional human sperm with higher DNA integrity and fewer reactive oxygen species
- Separation efficiency of a microfluidic sperm sorter to minimize sperm DNA damage
- Guidance and self‐sorting of active swimmers: 3D periodic arrays increase persistence length of human sperm selecting for the fittest
- Development and prospects of microfluidic platforms for sperm inspection
- Emerging technologies for home-based semen analysis
- Sperm quality assessment via separation and sedimentation in a microfluidic device
- Analysis of sperm concentration and motility in a microfluidic device
- Spermometer: electrical characterization of single boar sperm motility
- Development of computer-assisted sperm analysis plugin for analyzing sperm motion in microfluidic environments using Image‑J
Fill out the form below to talk to one of our experts, or ask about how to buy microfluidic devices:
Infertility is an ever-increasing public health concern. Microfluidics can enhance the assisted reproduction technologies.