Healthcare access around the world or lack thereof
While healthcare access has increased globally in the last three decades1, at least half the world still lacks access to essential healthcare services2. For the ones that do have access, the high costs can often push them towards extreme poverty, bankruptcies, and homelessness. While there is a direct correlation between income equality and access to healthcare, another major reason that access to healthcare remains elusive to half the world population is because of the multiple dimensions that constitute healthcare – awareness and access to information about healthcare, access to health services such as hospital, ambulance, diagnostics, medicines, trained doctors and nurses, life-saving treatments, follow-ups among several others. Covering most or all of these aspects simultaneously at a location can often be a challenging task.
Diagnostics and Microfluidics
Next to health awareness and immunizations, diagnostics are among the front liners in health services. The majority of the downstream healthcare decisions (and therefore costs) are dependent on timely and accurate diagnosis. As our understandings of human physiology and pathology have evolved, so have the diagnostic tools. Unlike lab testing which involved collecting samples from patients and transporting them to a distant laboratory and waiting to learn the results, point-of-care (POC) diagnostics have made medical testing possible at patient’s location in a much-reduced timeframe thus expediting medical decisions.
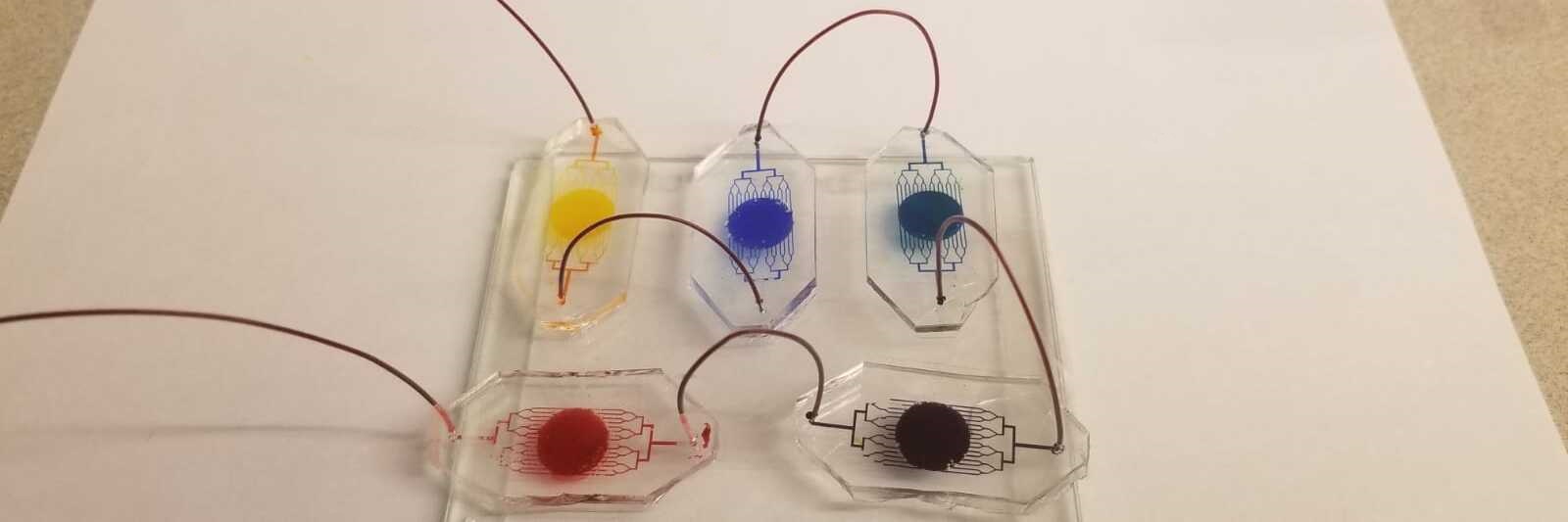
Microfluidic technologies have played a critical role in the rapid evolution of POC devices in the health industry. They offer numerous advantages: lower costs, reduced sample volumes, faster turn-around times, user-friendliness, device portability and high-throughput screening(HTS). Low costs and portability make it possible to adapt them in settings with limited or non-existent healthcare infrastructure. User-friendliness, easier result interpretations (such as through colorimetric assays) make it an attractive option in settings with limited or no access to trained health care providers.
Several companies have now successfully introduced microfluidic POC testing devices into the market. Several products have now made it to pharmacy shelves such as pregnancy tests and glucose monitoring kits. The global market for microfluidics was valued at 8.28 billion in 2017 and is expected to reach up to USD 27.91 billion by 20233. While the majority of the market for microfluidic devices is currently in developed countries, it is the developing countries where it can serve as a major game-changer. While cancers and cardiac diseases are the top killers in developed countries such as the US, infectious diseases, such as malaria, HIV/AIDS, and tuberculosis, are the leading cause of death in several developing nations. Current diagnostic procedures for these involve benchtop tests and assays with heavy reliability on instruments and reagents and are often time-consuming. With the focus shifting towards microfluidics, there have been several recent attempts to introduce microfluidics in developing nations. Several proof-of-concept studies have indeed shown that microfluidic POC devices can be a route to provide reliable and faster diagnostic services in these areas. Chin et al used a microfluidic device to detect HIV and syphilis in the Rwandan population using blood volumes as little as 1 μl and a turn-around time of 20 minutes4. Hugo et al. demonstrated the potential of a centrifugal microfluidic platform for POC diagnostic applications in South Africa5. Taylor et al showed the potential of PCR-on-chip device for malaria diagnosis among patient samples from Uganda6. Diagnostics For All, a non-profit started by Dr. George Whitesides and his group at Harvard, uses paper microfluidics for development of POC diagnostics for developing countries. Field studies have been conducted in Vietnam and Kenya7. Commercial companies that have microfluidic POC devices for infectious diseases include Alere, Trinity Biotech, and IMMY that use lateral flow immunoassay strips for the detection of diseases such as malaria, meningitis, filariasis, HIV, flu, and Legionnaire’s Disease. Alere, a market leader in this field, partners with several non-profits for the distribution of malaria and HIV testing POC kits in developing nations8.
Conclusion and future perspective
While enough studies and pilot projects have demonstrated the vast potential of microfluidics in the diagnosis of infectious diseases in a developing country, the target groups are way bigger than current reach of the microfluidic research and market. This calls for an action plan involving several stakeholders, such as the World Health Organization, governments, administrators, private companies, non-profits, and locals, to work in concert and collaborations. While mass-production will undoubtedly help meet the demands and lower the cost at the manufacturer and consumer ends, affordability will always remain a huge bottleneck in the widespread use of these devices in developing countries. Current efforts and successes have only been possible due to the involvement of non-profits. This issue further calls for bridging the gap between research and policy. Governments can play major roles here by introducing schemes and subsidies to increase the reach of the products.
There are innovations required on multiple fronts to tackle the issue of introducing microfluidic POC diagnostic devices to such a massive fraction of the world population. There is a need to ensure that material used for making these devices is readily available, safe, light-weight and well-suited for mass-production. The final devices also need to be handy and easy to transport. Technologies such as lab-on-a-drone9 need to be further advanced to ensure easy and wide distribution of these devices to remote areas. While the devices need to be user-friendly and must require minimal training, there should be provisions to store results and data for future use by integrating with everyday devices such as cell phones. Devices should also include multiple tests within the same setup to ensure high-throughput screening among populations plagued by multiple infections.
While the current issue at hand is focused on microfluidic-based affordable diagnostics for developing countries, microfluidics can play important roles even in health services downstream of diagnosis. Microfluidic organ-on-a-chip and human-on-a-chip platforms are promising technologies to advance precision medicines. Several drugs are known to have variable effects on different populations owing to genetic differences. Testing established drugs on organ-on-chip platforms based on cells from a certain sub-population can provide useful results in terms of predicting the safety of the introduction of drugs to that population. Furthermore, these platforms have also been touted as the future of novel drug development and toxicity testing.
While the field of microfluidics has now been around for 30 years, the technology still remains heavily confined to academia and basic research. Institutions and companies should now steer this field into practical real-world applications – providing healthcare access around the world being a major one due to the overwhelming size of the population that lacks basic healthcare. The low cost, low sample volumes, portability, reliability and faster turn-around times make it the most promising candidate for a tool that can bring diagnostics from bench to bedside.
References
1. https://medicalxpress.com/news/2018-05-global-healthcare-access-quality-.html
2. https://www.who.int/news-room/detail/13-12-2017-world-bank-and-who-half-the-world-lacks-access-to-essential-health-services-100-million-still-pushed-into-extreme-poverty-because-of-health-expenses
3. https://www.marketsandmarkets.com/Market-Reports/microfluidics-market-1305.html
4. Chin, C. D. et al. Microfluidics-based diagnostics of infectious diseases in the developing world. Nat. Med. 17, 1015–1019 (2011).
5. Hugo, S., Land, K., Madou, M. & Kido, H. A centrifugal microfluidic platform for point-of-care diagnostic applications. S. Afr. J. Sci. 110, (2014).
6. Taylor, B. J. et al. A lab-on-chip for malaria diagnosis and surveillance. Malar. J. 13, 179 (2014).
7. http://dfa.org/
8. https://www.alere.com/en/home/about/corporate-responsibility.html
9. Priye, A. et al. Lab-on-a-Drone: Toward Pinpoint Deployment of Smartphone-Enabled Nucleic Acid-Based Diagnostics for Mobile Health Care. Anal. Chem. 88, 4651–4660 (2016)
Enjoyed this article? Don’t forget to share.

Vardhman Kumar
Vardhman is a Ph.D. candidate in the Department of Biomedical Engineering at Duke University. His work in Prof. Shyni Varghese’s lab involves the development of microfluidic platforms for understanding the biophysics of development and diseases.