Innovations in microfluidic modelling of the human body have enabled medical researchers to study pathology to a level of accuracy and efficiency that was previously unattainable.
These ‘disease-on-chip’ models build on previous advances in organ-on-chip technology, creating devices that can model disease processes specific to each modelled organ. Notable disease-on-chip innovations include Kambez Benam and colleagues’ model of human lung inflammation, and the device mimicking arterial thrombosis created by Pedro Costa and collaborators at the Universities of Twente and Utrecht. The key advantage of disease-on-chip technology over conventional disease models is that it facilitates assays that are both physiologically relevant and high-throughput.
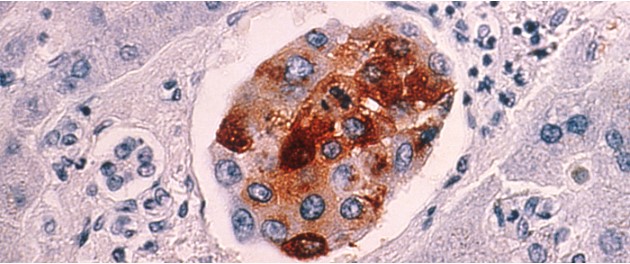
One particular area in which such advantages promise to have an enduring and significant impact is cancer biology, thanks to pioneering work done in modelling cancerous disease processes. Metastasis-on-chip is one such advance.
Metastasis: an Unsolved Problem
The majority of cancer-related deaths are due not to the formation of a single tumour, but rather the metastatic spread of cancerous cells around the body. Nonetheless, the processes underlying metastasis are still not well understood, despite the volumes of money contributed to cancer research (the National Cancer Institute in Washington alone has an operational budget of just under $5.4 billion). One major problem that has contributed to these failings is the ineffectiveness of current models. In vitro models are too abstracted and oversimplified to be reliable; a change as simple as altering the substrate on which cells are grown can produce contradictory data. Dish-based models also fail to provide physiological relevance, as accurately recreating the tumour microenvironment in two dimensions is challenging. Three-dimensional in vitro models are more complex, using scaffolds or matrices to form structures that more accurately replicate tumour structure. These models still struggle to recreate important environmental factors, such as surrounding vasculature. In vivo studies, which most commonly use rodent models, solve some of these problems, but throw up issues of their own, being extremely expensive and laborious. They also, more importantly, have a poor record of translation to clinical trials (roughly 8% of studies translate successfully).
Microfluidics: a Way Forward
Microfluidic devices have shown the potential to overcome these widespread problems. As the field is in its infancy, there remains a heterogeneity in the devices used to study metastasis, but the device created by Hossein Eslami Amirabad and colleagues to examine tumour cell migration is a representative example of devices commonly used (see below).

Metastasis on a chip. A top view (left) and exploded view (right) show a model of metastasis using a microfluidic chip. The top lower contains micro-chambers, separated from a bottom layer containing a microfluidic channel by a porous membrane.
Credit: Eslami Amirabadi, H., Luttge, R., & den Toonder, J. M. J. (2013). Cancer metastasis-on-a-chip.
Technische Universiteit Eindhoven
This device consists of two blocks, one studded with chambers representing organ sites, and a second block with a microfluidic channel running through it, representing a blood vessel. A porous PDMS membrane is placed between these blocks to act as a culture substrate, and tumour cells are then co-cultured into one of the organ chambers, alongside cells native to the organ being modelled. The invasion of neighbouring organs through the bloodstream can then be observed by tracking the tumour cells’ progress from the top block to the bottom block, and then back into the top block in a separate chamber. A similar system, modelling colonic cancer metastasis to the liver, was developed by Alexander Skardal and colleagues. This system was constructed using a hyaluronic acid-based hydrogel system, which could not only demonstrate the migratory capabilities of the tumour cells but also proved highly dynamic, allowing both pharmacological and mechanical manipulation. This introduction of extra layers of complexity and the easy modulation of such systems means that microfluidic devices have immense potential in this field of research. Devices investigating this process in more detail, focussing on individual tumour interactions, have also been created. This means that metastasis can be examined to a degree of precision simply not possible without microfluidic innovation.
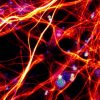
With such potential, one may ask what the next innovations in on-chip models will be. In a recent review, David Caballero and colleagues at the University of Minha suggest that integration with other technologies will allow the full benefits of microfluidics to be seen in tumour modelling. Integration of models with advanced imaging techniques, such as fluorescence or live-cell microscopy, could permit spatial and temporal modelling of tumours to a level of detail never before achieved. This integration has already shown potential in applications as broad as imaging vesicle trafficking and C. elegans larvae development. Microfluidics also will have a role to play in the emergence of personalized medical research. The genetic heterogeneity between metastatic tumours, even within a single patient, will require high-throughput but clinically relevant analysis techniques. Microfluidic pharmacological screening against these variable cancers will not only speed up care but will make the research process far more efficient and accurate.
Obstacles to achieving such lofty goals still remain. To make microfluidic devices more attractive as an alternative to current techniques, costs must be lowered, and links with existing technologies must be strengthened, with the aim of making microfluidics a technology that can be used across the healthcare industry, and that healthcare researchers actively seek out over more traditional and familiar techniques. Mohammed, Haswell, and Gibson argue in an excellent review of this area that innovators in microfluidic technology must consider the whole design and engineering process instead of simply the functionality of the end product. It is well and good to develop a device that allows superior tumour diagnostics, but if it is not cost-effective and not made will healthcare industry clients in mind, it will struggle to survive outside the lab of those who created it. Metastasis-on-chip technology, like many other medical microfluidic applications, has immense potential, but practicality and creativity are now required to realize that potential.
Enjoyed this article? Don’t forget to share.

RJ Mackenzie, MPhil
RJ is a science communicator and writer based in Glasgow, Scotland.