The liver is the largest internal organ in the human body, and it fuels equally large dilemmas. The quandary of the liver transplant system, when there is only one organ donor but two terminally ill people who need it, is this: how are decisions made about who lives and who will die? Who “deserves” a liver transplant more?
That’s the plot of the play Patience, which premiered in 2017 in Edinburgh. Inspired by actual patient experiences, Patience unravels the struggles facing decision-makers in the organ-transplant universe. Two women in need of a transplant, and the doctor who must decide which of them will get it, are the main characters. One patient is a young woman with autoimmune hepatitis, whose life is riddled with hospitalizations. The other is a recovering alcoholic.
The younger woman whose fate was the disease, and not bad choices around drunkenness, seems more deserving. But she upends expectations when she refuses to take steroids she needs to prepare for surgery— because they make her look fat. In contrast, the recovering alcoholic is desperate to do anything necessary to rehabilitate herself and her career in biochemistry. So by the time the decision is made, the audience feels sympathy for both patients.
Organoid advancement might make this theatrical plot obsolete. More thorough understanding of liver-stem-cell practicality may answer the question, who gets a new liver? And the answer might be — anyone who needs it.
Liver organoid progress may banish the concept of “deserving” to the history books. Liver failure is currently treatable only with transplants. More than one million patients worldwide die annually while waiting for donor livers, which are in short supply.
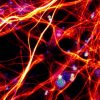
A 2017 U.S. National Institutes of Health hepatology study covers novel approaches to human liver organogenesis. The researchers identified signals that seem to regulate the differentiation of liver cells, by dissecting the mechanism of organoid formation. Innovations in their methodology point to personalized studies using patient-derived cells for disease and toxicology experiments.
Hans Cleversleads the Hubrecht Institute for Developmental Biology and Stem Cell Research, and is a professor of Molecular Genetics at The Netherlands’ University Medical Center in Utrecht. Over many years his team has innovated culturing methods for liver organoids. The Hubrechtteam has developed ways to culture a twin of a full-grown liver from a single liver stem cell. The tissue was genetically the same as healthy liver tissue and stable as well.
Printing, or more accurately “bioprinting” of 3D organoids, turns cells from human donor organs into bio-ink, to generate— or bioprint — liver organoids. Such liver organoids can be used to test drug safety. The UK’s Medical Research Council is spearheading the generation of 3D liver tissue to treat chronic liver disease, by developing 3D implantable organoids. In the U.S., in December 2017, the Food and Drug Administration granted special status to the Organovo company to treat a rare genetic deficiency, utilizing 3D-bioprinted liver tissue.
Dr. Meritxell Huch at the UK’s University of Cambridge has worked with Clevers to develop culture methods for obtaining liver organoids. Her team researches organoids that replicate original pathophysiology of liver tumours. They focus on retaining tissue function and genetic stability. This preserves aspects of the original tumor, enabling discrimination between various tumor tissues for analysis. These organoids led to the identification of a potential therapy for liver cancer. The organoids that the Huch and Clevers teams develop are furthering the understanding of liver cancer biology and developing personalized medicine approaches.
A*STAR’s Genome Institute of Singapore (GIS) and Institute of Molecular and Cellular Biology (IMCB), in collaboration with the Stanford University School of Medicine, is also investigating the generation of liver cells from stem cells to treat liver failure. Dr. Ng Huck Hui, Executive Director of GIS, explains the project: “The ability to generate large quantities of stem-cell derived liver cells holds the potential to sustain patients with liver failure while they await a full liver transplant.
“This holds great promise for helping to improve patient survival rates and alleviating the burden of liver failure on societies.”
That would be welcome by liver patients and their families.
There is no spoiler alert in this blog. The ending of the play Patience won’t be revealed. The play “deserves” to be seen — even if functional organoid research makes it irrelevant.
Enjoyed this article? Don’t forget to share.

Kathy Jean Schultz
Kathy Jean Schultz is a freelance medical science writer who focuses on medical innovations. She earned a Master’s Degree in Research Methodology from Hofstra University, and a Master’s Degree in Psychology from Long Island University. She is a member of the National Association of Science Writers, and the Association of Health Care Journalists. Her articles about organoids include "Would you trust a 3-D printed mini organ to test your drugs?" and "Stem cells not only slow disease, they come with their own safety test".