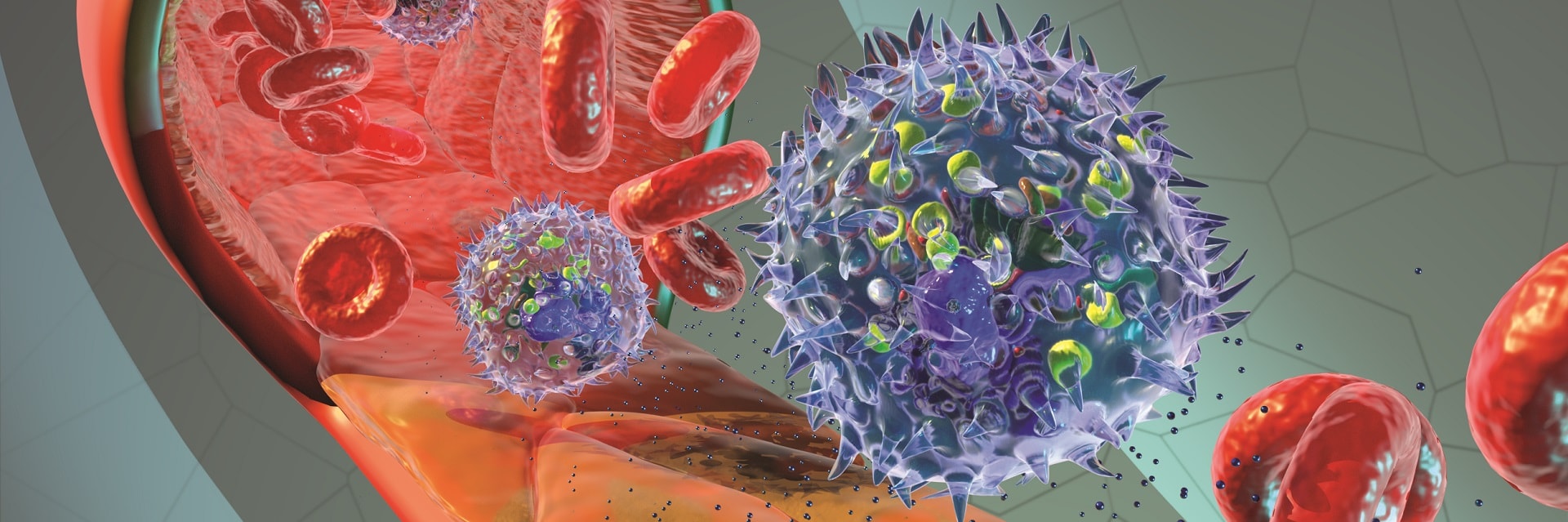
In a recent special communication edition of The Journal of the American Medical Association, sepsis was defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection1. This definition highlights the devastating nature of sepsis; arising from a simple infection and spiralling to an uncontrolled and often fatal immune response. Recent epidemiological studies place sepsis mortality at a staggering 18%, making it the leading cause of death in intensive care units2. This amounts to more than 30 million cases globally each year, nearly 6 million of which ending in the patient death [who.int]. Following largely disappointing and exceedingly expensive efforts in the development of sepsis-specific therapies, treatment of patients suffering from sepsis is left to clinical management of associated symptoms. Additionally, timely diagnosis of sepsis is imperative for effective treatment, however, most patients are presented to the clinic in an advanced, deteriorated state of disease. These substantial setbacks in the progression of sepsis treatment lead us to two major questions:
- How do we cost-effectively and accurately screen potential sepsis pharmaceuticals?
- Can we diagnose sepsis patients earlier to permit corrective intervention before irreversible disease progression?
We believe microfluidics can help answer these questions.
In the pursuit of developing a single, manufacturable system to answer our outstanding questions in sepsis research, we add an additional question to the problem: how can the field of microfluidics overcome the implicit challenges faced when bridging basic science research and clinical application? It is clear that communication between the research lab and the clinic (a field often referred to as translational biomedical science) can have an immediate impact on the health care system and in the context of sepsis, this increased dialogue has left a profound mark on the disease.
Microfluidics and Sepsis Research
Since the rise of conventional polydimethylsiloxane (PDMS) based microfluidic devices in the late 1990s and early 2000s, production of microphysiological systems (MPS) for a broad range of applications has increased, while the cost associated with these devices has declined. This large-scale development means that MPS are no longer primarily restricted to the labs of engineers and are now reaching the hands of knowledgeable biologists. From whole organ mimetics to blood-brain barrier models, microfluidic devices open the door to highly controlled studies on human cell lines and associated clinical samples. What is lost in physiological accuracy, is gained in simplicity and reproducibility, allowing for often complex or even unimaginable studies (when performed in vivo) at the lab bench. These points are emphasized in the context of sepsis research due to the following:
- Previous studies in murine (a.k.a. mouse and rat) models of sepsis have highlighted important physiological differences between these experimental species and what really occurs in humans, particularly in the pathologic immune response defining the disease3.
- Mass failure of immune-modulating drugs for the treatment of sepsis and the large financial burden associated with those shortcomings means labs are acutely aware of the need for cost-effective ways to screen for future therapeutics
For these reasons, microfluidics is a very attractive tool for sepsis research. In Dr. James McGrath’s lab at the University of Rochester, we utilize microfluidic devices to mimic the inflamed microvasculature related to sepsis pathophysiology and investigate the relationship between white blood cells (neutrophils) and the endothelial cells that line the vascular wall (Movie 1)4. The systems used herein, and others alike, allow for the highly controlled and meticulous study of the immune response in sepsis, all aimed at developing a better understanding of the disease, with the future hope of a cure. In doing so, we can maintain a significantly lower price point compared to studies performed in murine models.
Across the field, ‘lab-on-a-chip’ microfluidic systems are being exploited for drug discovery in all aspects of human disease because of their inherent controllable properties and low cost. These efforts were reviewed previously in Nature Drug Discovery5.
Movie 1. In our lab, microfluidic devices are assembled in a layer-by-layer fashion, allowing for human endothelial cell culture on a silicon nanomembrane (green/yellow chip). The resulting microvascular mimetics facilitate a live microscopy study of the white blood cell-lead immune response. The final frame depicts the nanoporous membrane utilized as the endothelial cell culture support.
Microfluidics in the Clinic
With low production costs, facile use, and increased throughput, microfluidic devices have left the confines of basic science research and entered the mainstream of clinical translation. Receiving major attention in a January 2019 issue of National Geographic, ‘lab-on-a-chip’ devices are highlighted as ‘the future of medicine’, with emphasis on the potential for personalized medicine. By incorporating patient cells and fluid samples to a specialized device, personalized medicine can permit patient-specific therapy and guided pharmaceuticals. Additionally, the requirement of minute sample volumes allows for increased experimentation/diagnostics on often precious patient samples or expensive reagents. These benefits have already proven impactful to the sepsis community: In a 2018 issue of Nature Biomedical Engineering, Ellett and colleagues describe a microfluidic platform that analyzes patient blood cell (neutrophil) motility to accurately diagnoses sepsis6. The device used immediately showcases the benefits of microfluidics in the clinic, as the diagnosis is performed using a single drop of blood, eliminating the need for large volume venipuncture draws or post-draw processing. In our lab, we are working on translating our MPS, namely, a stem cell-based mimetic of the blood-brain barrier, to act as an early-stage sepsis diagnostic. In addition to diagnostics, microfluidics has been suggested as an avenue to drugless sepsis treatment. Since the 1990s, it has been hypothesized that membrane-based, low footprint microfluidic devices may facilitate a process termed extracorporeal blood purification; a procedure in which harmful inflammatory factors are continuously filtered out of the blood, halting the maladaptive immune response. Given the applications presented here, the potential for impactful microfluidic technologies in the clinic is clear.
Bridging the Gap
As interest peaks in the use of microfluidics in the clinic, the question remains: how do we translate often meticulous device manufacturing to large scale production? This fabrication dilemma is most likely the demise of many microfluidic technologies developed in the lab. What is routine at a small scale in the cleanroom, may not be feasible at the necessary volumes to launch microfluidic devices into the clinic. Because of these concerns, many labs and clinics are less willing to adopt microfluidics in their work.
So how do we change this environment? Based on our recent experience, we suggest the following:
- Design devices that may be used for a variety of applications (simplicity and functionality is key)
- Work closely with microfluidics companies to adjust your designs for higher volume production goals
- Involve other labs that work on similar products to share the benefits of these platforms
- Talk to clinicians that would handle these devices to understand what problems are most important to them
In conclusion, microfluidics has the ability to open the door to truly translational science. In a single device, one can study the disease mechanism, develop targeted drugs, and diagnose patients. These multidisciplinary platforms effectively narrow the gap between basic science research and the clinic, paving the way to a future with a direct line of communication, from the patient straight to the lab.
References
1. Singer, M., Deutschman, C. S., Seymour, C. & et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA315, 801-810, doi:10.1001/jama.2016.0287 (2016).
2. Gotts, J. E. & Matthay, M. A. Sepsis: pathophysiology and clinical management. BMJ353, i1585, doi:10.1136/bmj.i1585 (2016).
3. Rittirsch, D., Hoesel, L. M. & Ward, P. A. The disconnect between animal models of sepsis and human sepsis. J Leukoc Biol81, 137-143, doi:10.1189/jlb.0806542 (2007).
4. Salminen, A. T. et al. Ultrathin Dual-Scale Nano- and Microporous Membranes for Vascular Transmigration Models. Small15, e1804111, doi:10.1002/smll.201804111 (2019).
5. Dittrich, P. S. & Manz, A. Lab-on-a-chip: microfluidics in drug discovery. Nat Rev Drug Discov5, 210-218, doi:10.1038/nrd1985 (2006).
6. Ellett, F. et al. Diagnosis of sepsis from a drop of blood by measurement of spontaneous neutrophil motility in a microfluidic assay. Nature Biomedical Engineering2, 207-214, doi:10.1038/s41551-018-0208-z (2018).
Enjoyed this article? Don’t forget to share.

Alec Salminen
Alec Salminen is a Ph.D. candidate in the Department of Biomedical Engineering at the University of Rochester. His work, under Dr. James McGrath, involves the fabrication of silicon nanomembranes and microfluidic mimetics of the microvasculature to study the innate immune response in sepsis. Additionally, Alec works with a microfluidic manufacturer to fabricate devices for a variety of applications, including an early-stage sepsis diagnostic.
Elysia Masters, a Ph.D. candidate in the Department of Biomedical Engineering at the University of Rochester, aided in the writing of this post. More information on her work can be found below.